Polycystic Ovary Syndrome (PCOS) is often thought of as a condition that primarily affects younger women, but its impact doesn’t end there. As more people with PCOS enter perimenopause and menopause, research is shedding light on how symptoms and risks change, and what steps you can take to protect your health during this important stage of life.
What Is PCOS?
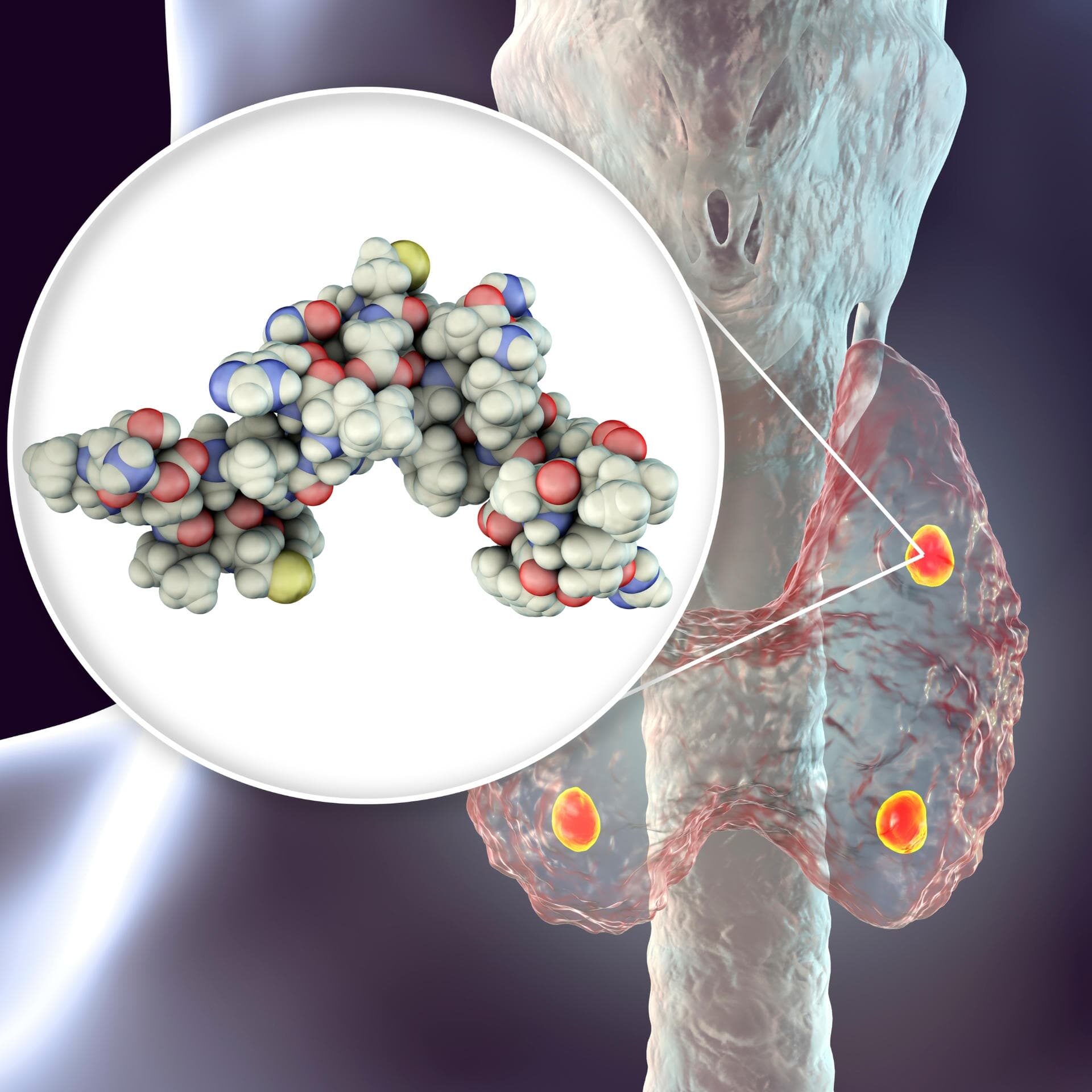
PCOS is a hormonal disorder that affects how the ovaries work. It often leads to irregular or missed periods, higher levels of male-type hormones (androgens), and insulin resistance. Many women experience symptoms such as acne, increased facial or body hair, fertility challenges, and weight gain. Importantly, PCOS is a lifelong condition—it does not simply go away with age or once menstruation stops.
What Happens During Perimenopause and Menopause
Perimenopause is the transitional period before menopause when estrogen and progesterone levels begin to fluctuate. This stage can last for several years and is often marked by irregular cycles, hot flashes, and mood changes. Menopause, on the other hand, is defined as 12 consecutive months without a menstrual period and signals the end of natural ovarian hormone production.
Research shows that women with PCOS often reach menopause a little later than average—sometimes one to two years later. Because symptoms like irregular periods, weight gain, and changes in skin or mood can occur with both PCOS and perimenopause, it can be difficult to tell which condition is driving the changes you may be experiencing.
How PCOS Changes with Menopause
While menstrual irregularities resolve once menopause begins, PCOS does not disappear. In fact, the focus shifts toward long-term health risks. Women with PCOS continue to face a higher risk of insulin resistance, type 2 diabetes, high cholesterol, and cardiovascular disease. Some symptoms of androgen excess, such as acne or hair growth, may improve, but for many women, they persist even after menopause.
Managing PCOS Through Menopause
Here are practical steps for managing PCOS and menopause together, especially to reduce risks and improve quality of life:
- Lifestyle
- Maintain a healthy weight through balanced nutrition (with whole foods, lean protein, plenty of fiber) and regular physical activity.
- Focus on good sleep hygiene and stress management—both affect hormones.
- Avoid smoking; alcohol in moderation.
- Hormonal & Medical Treatments
- Hormone therapy (if appropriate) to address menopausal symptoms.
- Medications to manage insulin resistance (e.g. metformin) or regulate androgen levels.
- Regular monitoring of lipids, blood sugar, and blood pressure.
- Regular Check-ups
- See your endocrinologist or health provider to review labs and symptoms at least annually.
- Screen for diabetes, heart disease, and other metabolic complications.
- Be Proactive
- Work with your care team (endocrinologist, gynecologist, primary care) to tailor a plan based on how PCOS has affected you through your life.
Contact Texas Diabetes
If you have PCOS and are approaching perimenopause or already navigating menopause, Texas Diabetes is here to help. Our endocrinologists specialize in managing hormone changes, metabolic health, and long-term risks to ensure you receive the comprehensive care you deserve.
If you’d like to schedule an appointment with one of our endocrinologists at Texas Diabetes & Endocrinology, please contact us at (512) 458-8400 or request an appointment online.