Thyroid. For many of us, the word conjures up a sense of curiosity, wonderment, even awe! What is the thyroid gland and what exactly does it do? How do you know if you’ve got a thyroid problem?
Let’s start with the basics. The thyroid gland is a small, butterfly shaped gland that sits in the base of your neck. It makes thyroid hormones (thyroxine and triiodothyronine) which regulate your metabolism. Metabolism is a series of processes that control how your body creates and uses energy. So…why do we hear so much about thyroid and thyroid dysfunction? Well, it turns out that there are some pretty common illnesses that can affect thyroid health.
A thyroid hormone deficiency is a state called HYPOTHYROIDISM. You may have this if your thyroid gland is the target of an autoimmune attack (this is called Hashimoto’s disease) or if you’ve had your thyroid gland irradiated or surgically removed. Since thyroid hormone is your source of metabolism, untreated hypothyroidism can cause a multitude of symptoms: fatigue, lethargy, weight gain, dry skin, depression, constipation, hair loss, cold intolerance, irregular menstrual cycles in women-these are all symptoms of slowed metabolism. The solution is simple-take thyroid hormone replacement which comes as an oral supplement.
A thyroid hormone excess is a state called HYPERTHYROIDISM. You may have this if your gland is the target of an autoimmune attack (this is called Graves disease) or if you thyroid gland grows renegade chunks of thyroid tissue that lose the ability to regulate the amount of thyroid hormone they produce. These so called “hot nodules” manufacture extra thyroid hormone without your body’s permission. Finally, you can develop hyperthyroidism if your thyroid gland becomes acutely injured – an injured thyroid gland sheds pre-formed thyroid hormone. This is called a thyroiditis. Medications, autoimmune attacks, viruses and pregnancy can cause thyroiditis. Hyperthyroidism can also cause of multitude of symptoms: rapid heart rate, weight loss, tremors, palpitations, frequent and loose stools, anxiety, irregular menstrual cycles in women-these are all symptoms of accelerated metabolism. The solution is not quite as straightforward as it is for a hypothyroid state but a hyperthyroid state can certainly be treated. Depending on the underlying cause, a hyperthyroid state can be treated with surgery (removal of the thyroid gland), medications, or irradiation. In some cases of thyroiditis, the thyroid gland heals on its own.
The thyroid gland is also prone to structural illnesses. Thyroid glands often grow NODULES – a thyroid nodule is an abnormal growth of thyroid cells that forms a lump within the thyroid gland. While the vast majority of nodules (probably more than 95%) are benign, some nodules do contain cancers within them so timely evaluation is important. Thyroid ultrasound is an important tool used to assess nodule size and characteristics. If necessary, a thyroid fine needle aspiration biopsy can be done to assess the potential for malignancy. This is a relatively easy and straightforward procedure that can done in the physician’s office with the aid of an ultrasound machine.
Finally…a word about thyroid hormone replacement. Oral thyroid hormone supplementation comes in various forms:
One synthetic version of thyroid hormone is called Levothyroxine-this is synthetic thyroxine also known as T4. There are several branded versions of Levothyroxine: Synthroid, Levoxyl, Unithroid, Tirosint are some common ones. Generally speaking, branded levothyroxine preparations are usually consistent in terms of potency from batch to batch. Generic formulations may not be as consistent so your provider may specify a branded version.
Another synthetic version of thyroid hormone is called Liothyronine. This is synthetic triiodothyronine also known as T3. The most common branded version of Liothyronine is called Cytomel. Liothyronine is absorbed in a more rapid fashion and some patients report an increased sense of well-being when it is used in combination with Levothyroxine. Although the guidelines published by the ATA (American Thyroid Association) conclude that Levothyroxine should remain the standard of treatment for hypothyroidism, many physicians do prescribe combination therapy with Levothyroxine and Liothyronine in patients who may not feel as well on Levothyroxine monotherapy.
The nonsynthetic version of thyroid hormone is dessicated animal thyroid extract. This is exactly what it sounds like-it’s thyroid hormone extracted from the thyroid glands of animals-most commonly, pigs. Animal thyroid extracts were first used to treat hypothyroidism in the late 19th century but became largely replaced by synthetic versions. One concern: animal thyroid extracts have more T3 in relation to T4 compared to the ratio produced by a healthy human gland. T3 may place a more potent metabolic demand on the heart and in some individuals can precipitate dangerous heart rhythms. For this reason, your provider may be reluctant to prescribe this type of thyroid hormone if you are older and/or have an underlying heart condition.
In addition to thyroid health, there are numerous factors that contribute to a person’s physical and mental sense of well-being, or lack thereof. Among these factors: diet and sleep patterns, coexisting disease states, relationships with other human beings, the quality of the surrounding environment, the ability to navigate stress, etc…. When we feel unwell, we are best served to step back and take a look at the big picture. Because while the thyroid gland is indeed a powerful factory of thyroid hormone production and thyroid hormone itself is an incredibly capable hormone, the thyroid is only one small part of a much more complex and sophisticated piece of machinery we call the human body.
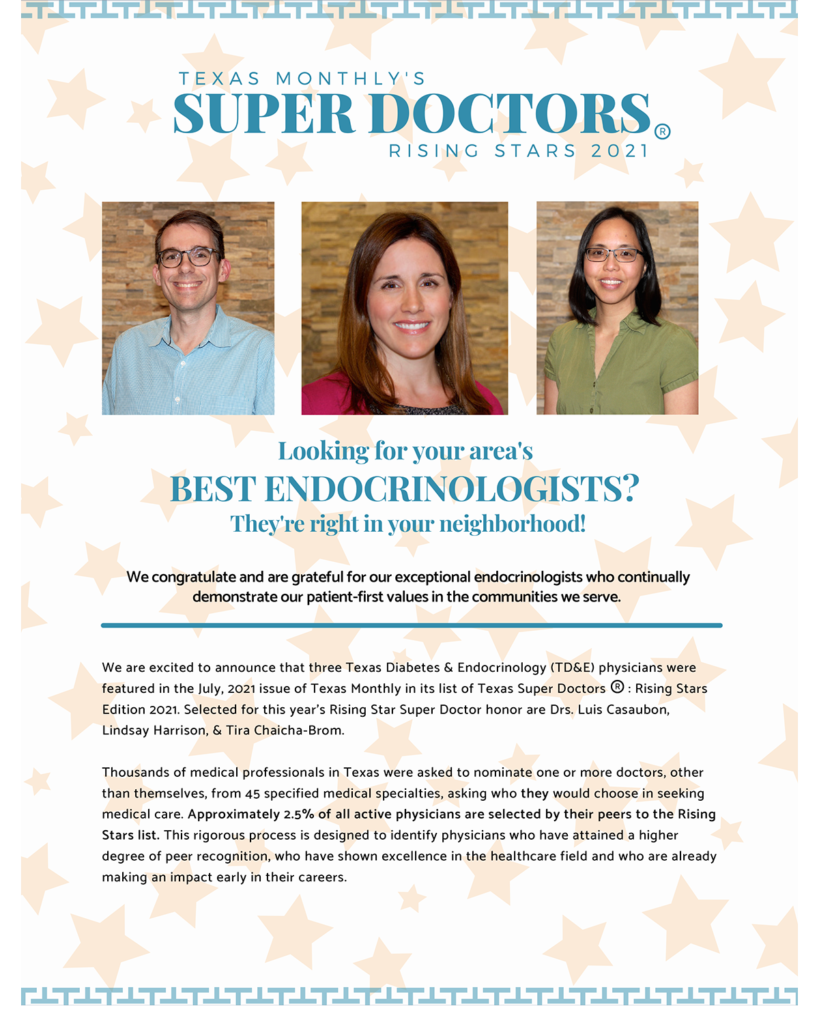
If you have been thinking of having your thyroid levels checked out the endocrinologists at Texas Diabetes can help walk you through the process. When you trust Texas Diabetes & Endocrinology with your thyroid condition, you are assigned your own, personal team of carers who will get to know you and tailor a treatment plan that fits your individual needs.
Schedule your appointment with us today.