The Food and Drug Administration (FDA) has approved Tymlos (abaloparatide) injection for the treatment of postmenopausal women with osteoporosis at high risk for fracture. High risk for fracture is defined as history of osteoporotic fracture, multiple risk factors for fracture, or patients who have failed or are intolerant to other available osteoporosis therapy. In postmenopausal women with osteoporosis, Tymlos reduces the risk of vertebral and nonvertebral fractures.
Clinical Data
The FDA’s approval of Tymlos was based on results from the ACTIVE trial and an extension of this trial. These studies demonstrated significant reductions in the risk of vertebral and nonvertebral fractures regardless of age, years since menopause, presence or absence of prior fracture and bone mineral density (BMD) at baseline. In clinical studies, Tymlos reduced the incidence of new vertebral and nonvertebral fractures, and increased bone mineral density (BMD).
The results from the ACTIVE trial were published in the Journal of the American Medical Association in August of 2016, and the results of the first six months of ACTIVExtend were published in the Mayo Clinic Proceedings in February 2017.
Specifically, in the ACTIVE trial, TYMLOS demonstrated significant reductions in the relative risk of new vertebral and nonvertebral fractures compared to placebo in the ACTIVE trial of:
- 86% in new vertebral fractures
- 43% in nonvertebral fractures
The absolute risk reductions were 3.6% and 2.0%, respectively.
Safety information
Abaloparatide caused a dose-dependent increase in the incidence of osteosarcoma (a malignant bone tumor) in male and female rats. The effect was observed at systemic exposures to abaloparatide ranging from 4 to 28 times the exposure in humans receiving the 80 mcg dose. It is unknown if Tymlos will cause osteosarcoma in humans.
For this reason, the use of Tymlos is not recommended in patients at increased risk of osteosarcoma including those with Paget’s disease of bone or unexplained elevations of alkaline phosphatase, open epiphyses, bone metastases or skeletal malignancies, hereditary disorders predisposing to osteosarcoma, or prior external beam or implant radiation therapy involving the skeleton.
Adverse Reactions: The most common adverse reactions (incidence ≥2%) are hypercalcemia, hypercalciuria, dizziness, nausea, headache, palpitations, fatigue, upper abdominal pain and vertigo.
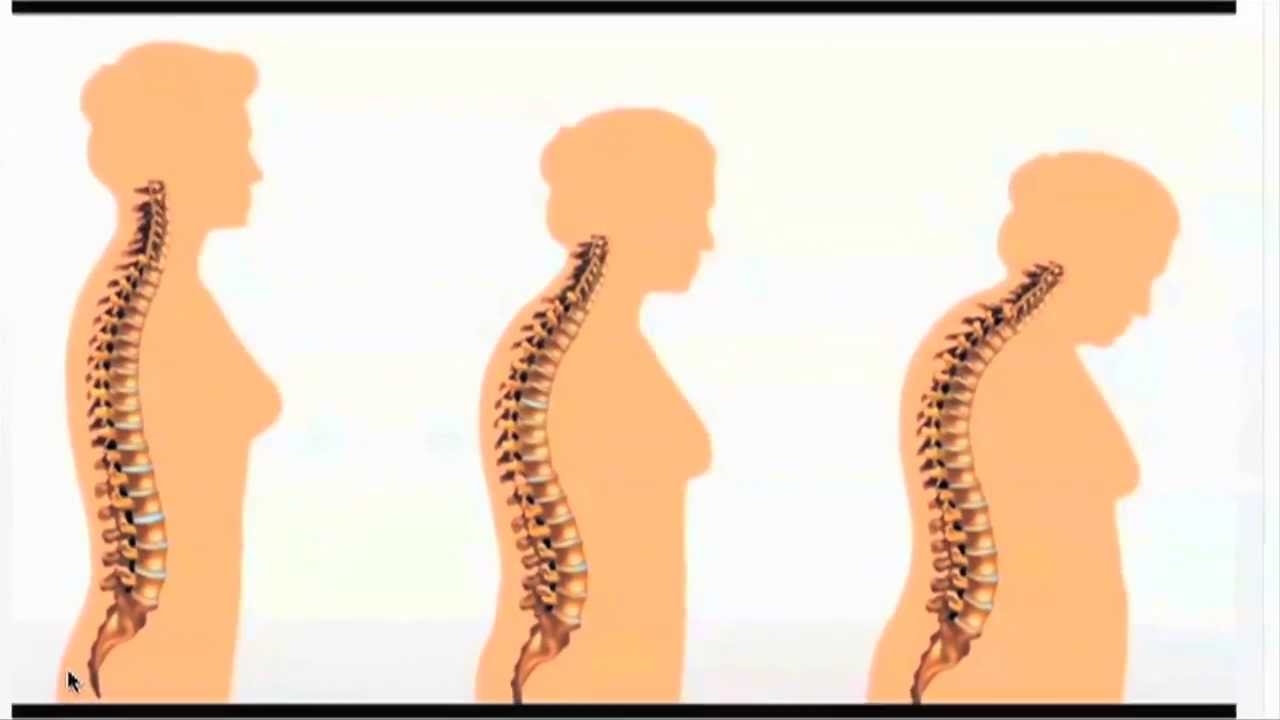
Reminders About Osteoporosis
Osteoporosis is a silent disease, often displaying no signs or symptoms until a fracture occurs, leaving the majority of people with osteoporosis undiagnosed and untreated. Osteoporotic fractures create a significant healthcare burden. An estimated two million osteoporotic fractures occur annually in the United States, and this number is projected to grow to three million by 2025.
The National Osteoporosis Foundation (NOF) has estimated that eight million women already have osteoporosis, and another approximately 44 million may have low bone mass placing them at increased risk for osteoporosis
Screening is key to diagnose osteoporosis. Once osteoporosis is diagnosed, it is very important to undergo a thorough evaluation to look at secondary factors that can contribute to osteoporosis. Once the evaluation is complete, you and your physician can review the best treatment plan for you.