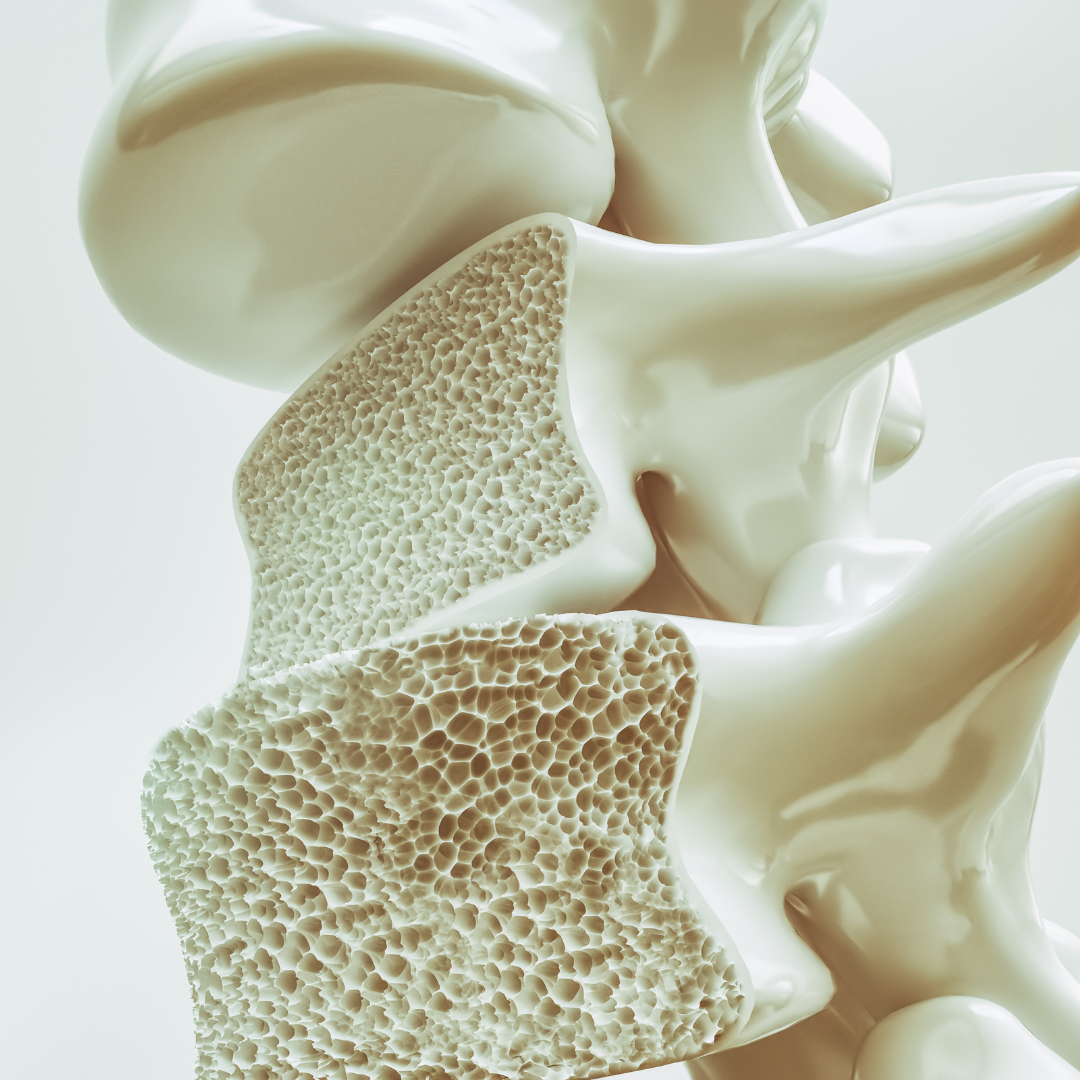
May is Osteoporosis Awareness Month. This condition, marked by severely weakened bones, is one that our board-certified endocrinologists treat daily here at Texas Diabetes & Endocrinology (TD&E).
While it is commonly known that calcium helps to strengthen bones and protect against osteoporosis, new research shows that good gut health (or the gut biome) can also play a large role in osteoporosis prevention and boosting bone density (the amount of minerals stored in bones to make them strong).
The gut biome is the complex mix of microorganisms that live in the body’s intestines and helps with immunity and food processing.
What is the connection between osteoporosis and the gut biome?
A new study recently published strongly supports previous findings that a healthy gut biome can in fact improve bone density and help protect against osteoporosis. This important connection between the gut biome and the body’s bones is known as the gut-bone axis.
Data shows that eating fruits and vegetables high in Vitamin C can increase production of the bone-making cells that protect them from weakening, or possibly fracturing and breaking, which is typically associated with osteoporosis. This conversion of Vitamin C into powerful bone-boosting cells takes place in the gut.
Research also continues to show that foods rich in calcium (like dairy products) and high in protein (lean meats and legumes) help to fortify bones and keep them strong.
Additionally, tracking certain types of bacteria that exist in the gut biome, and then supplementing with lacking bacteria known to boost bone-making cells, may become an increasingly more common option for osteoporosis prevention. This can be facilitated by a physician recommending a mix of synbiotics (probiotics combined with prebiotics) to promote healthy bacteria in your gut biome.
According to TD&E endocrinologist Dr. Mauli Shah, along with keeping your gut check in health, other ways you can help prevent osteoporosis are with “regular exercise (weight bearing or resistance exercises are best), and taking Vitamin D and calcium supplements.”
When should you see a doctor for osteoporosis?
Dr. Shah offers the following recommendations for when you should visit a doctor, or endocrinology expert, regarding your risk for osteoporosis:
- All women 65 years of age and older
- Post-menopausal women with certain risk factors, such as those who’ve had a previous fracture or been treated with steroids
- People who have a family history of osteoporosis or hip fractures
- People with rheumatoid arthritis
- Women who have entered premature menopause or men with low testosterone
Osteoporosis Treatment at Texas Diabetes
Our endocrinology and osteoporosis experts will help develop the right treatment plan for you to address your unique bone health needs. We typically recommend lifestyle modifications to start, like getting more exercise and eating well. Then we’ll determine what combination of dietary supplements, medications, and/or injections and IV infusions are best suited to protect and strengthen your bones.
Contact Us to Help Manage your Osteoporosis, Diabetes and Thyroid Conditions
If you’d like to schedule an appointment with one of our specialists at Texas Diabetes & Endocrinology and discover how our diabetes services and other endocrinology therapies can help you lead a full and active life, please contact us at (512) 458-8400 or request an appointment online.
Don’t forget to follow us on Facebook and Instagram and check back with us each month as we provide you helpful wellness and health information.