The CDC estimates that more than 29 million American adults are currently living with diabetes.
Diabetes is a chronic disease that affects how your body makes and processes glucose, or blood sugar. While it is possible to lead a very full and active life with diabetes if your diet and medications/insulin are carefully managed, there is still the potential for serious complications to occur.
What are some common diabetes complications?
Diabetes complications usually develop gradually over time with the disease. It is important to monitor your blood glucose levels vigilantly and stay on track regarding regular check-ups with your endocrinologist.
Some of the most common diabetes complications that our endocrinology experts see include:
- Heart disease: diabetics are twice as more likely to suffer from heart disease and stroke than others due to damaged blood vessels and nerves surrounding the heart
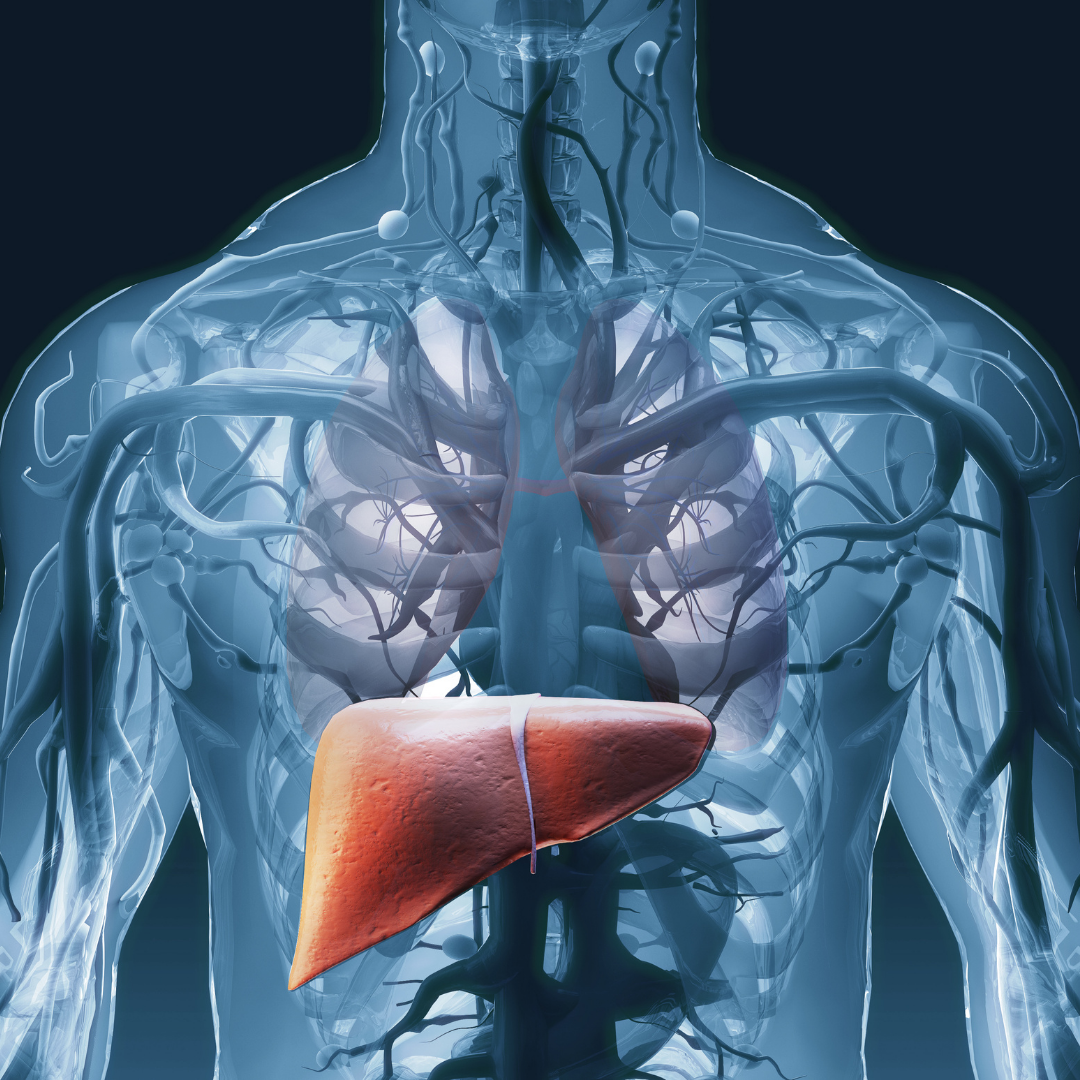
- Kidney disease: elevated blood sugar levels over time can lead to chronic kidney disease, the need for dialysis, and even kidney failure
- Blindness and eye issues: diabetes can also damage blood vessels in the eye/retina (diabetic retinopathy)
- Neuropathy: diabetic neuropathy, or nerve damage, is pain or numbness that stems from blood vessels and nerves (typically in the legs and feet) lacking sufficient oxygen or nutrients hijacked by high blood sugar
- Non-healing foot and leg ulcers: sores and infections that appear on the legs or feet due to poor circulation and elevated glucose levels can be hard to treat and may lead to amputation in extreme cases
If you notice signs or symptoms of any of these diabetes complications, speak with your endocrinologist right away about solutions to treat and manage them effectively.
Decreasing Your Risk for Diabetes Complications
Along with keeping regularly scheduled appointments with your physician, and taking medications/insulin as instructed, here are five other ways to help prevent from developing severe diabetes complications:
1. Follow a healthy diet of lean proteins, brightly colored fruits and vegetables, and whole grains.
2. Exercise regularly and aim for at least 150 minutes of physical activity per week.
3. Maintain a healthy weight and BMI (Body Mass Index) and speak to your doctor about what that optimal weight should be.
4. Manage your blood pressure and cholesterol levels and make sure they are within healthy and normal ranges.
5. Stop smoking to avoid additional damage to your heart and lungs beyond what high blood sugar levels may already contribute.
With proper management, and prompt attention to any symptoms you are experiencing, you can keep your diabetes complications to a minimum.
Contact Us to Help Manage your Diabetes, Osteoporosis and Thyroid Conditions
If you’d like to schedule an appointment with one of our endocrinology specialists in Austin or Round Rock please contact us at (512) 458-8400 or request an appointment online.
Don’t forget to follow us on Facebook and Instagram and check back with us each month as we provide you helpful wellness and health information.