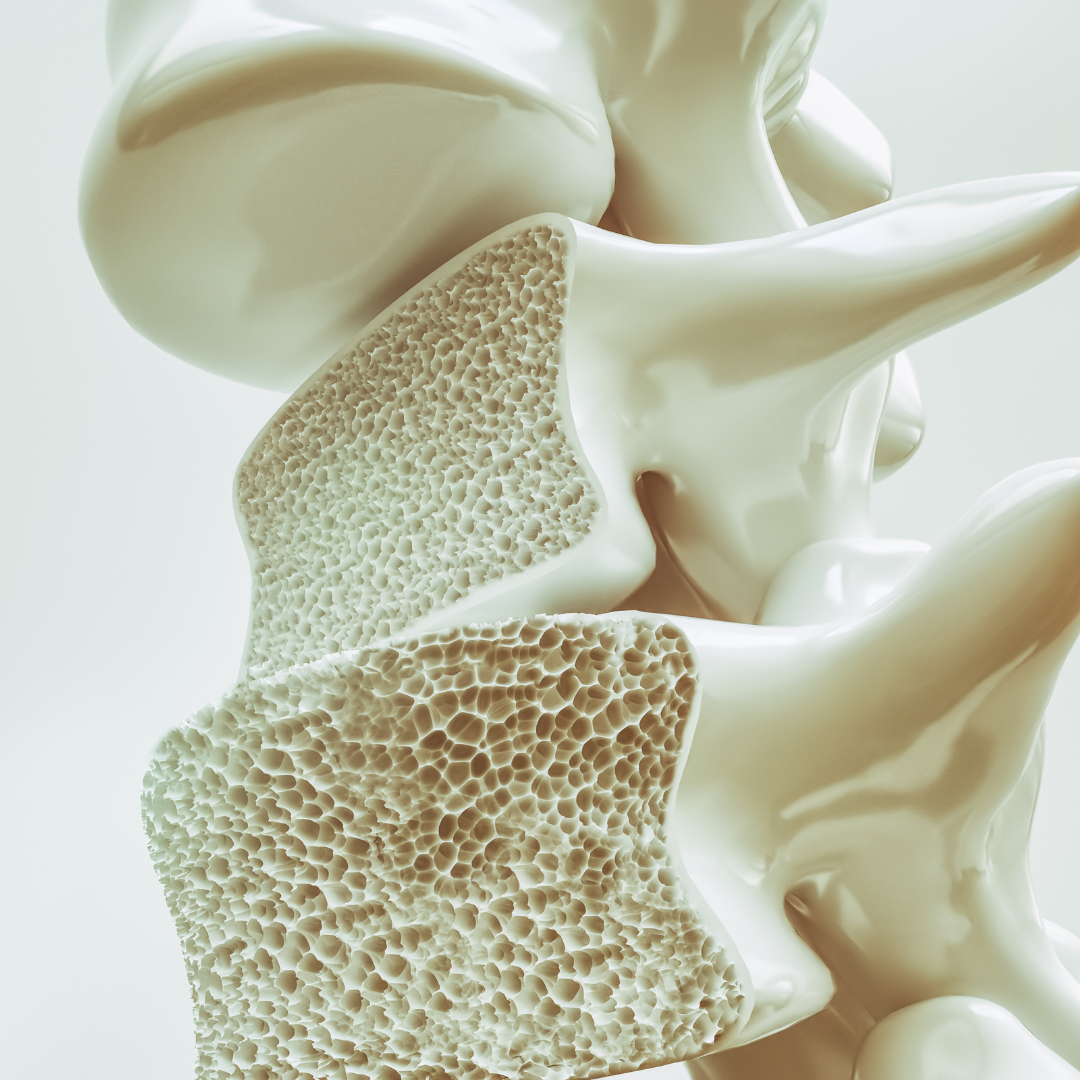
Osteoporosis is a common and potentially debilitating disease that affects an estimated 54 million Americans. Often referred to as a silent disease, osteoporosis can progress with no symptoms or warning signs until a fracture occurs. At Texas Diabetes and Endocrinology, we believe that preventing bone fractures is a priority.
In honor of Osteoporosis Awareness and Prevention Month, endocrinologist Dr. Keta Pandit is sharing everything you need to know about the condition.
What are the most common signs of osteoporosis?
Osteoporosis is characterized by low bone mass that results in microarchitectural disruption which causes decreased bone strength and increased risk of fracture. Some people may develop small microfractures in the vertebral spine, which may result in loss of height or hunched posture, known as kyphosis. Unfortunately, osteoporosis has no clinical manifestations until there is a fracture.
What risk factors raise a person’s chances of getting osteoporosis?
Women are much more likely to develop osteoporosis compared to men. Upon menopause women are not exposed to Estrogen, which is responsible for promoting bone growth. Therefore, postmenopausal women are at an increased risk of getting osteoporosis. Those with a family history of hip fractures or osteoporosis are also at an increased risk and should inform their doctor so that screening can be done appropriately.
Other factors that can increase osteoporosis risk can include:
- smoking
- daily use of alcohol
- history of steroid use
- early menopause in women
- low testosterone in men
- excessive use of thyroid hormones or history of hyperthyroidism
- hypercalciuria
- chronic medical conditions like diabetes and HIV
At what age should patients start thinking about osteoporosis prevention?
The National Bone Health & Osteoporosis Foundation (NBOF) and the U.S. Preventive Services Task Force(USPSTF) both recommend screening for osteoporosis in women of age 65 and above. NBOF also recommends screening early for all postmenopausal women with known risk factors. Regardless, all women of postmenopausal age are recommended to have adequate calcium and vitamin D to prevent bone loss.
For men, the recommendations have varied. NBOF recommends screening for all men over age 70 and as early as 50 years or older for men with risk factors. On the other hand, USPSTF has not provided a set guidance for what age men should be screened for osteoporosis.
What is one of the most common misconceptions patients have about osteoporosis?
One of the most common misconceptions about osteoporosis is that it presents pain in your bones or joints. Osteoporosis is a silent disease, and it does not present with any pain, unless there is a fracture or a bone deformity that comes from a previous history of fracture.
Many people believe that adequate intake of dairy in their diet is sufficient to prevent bone loss. However, you may not necessarily have adequate calcium despite daily use of dairy products.
Does osteoporosis affect men and women differently?
Women tend to have younger onset of bone loss and lose bone at a faster rate compared to men. Estrogen deficiency plays an important role in osteoporosis development, which is one of the factors that makes women more susceptible to osteoporosis compared to men.
How can someone best protect themselves from osteoporosis?
Prevention of osteoporosis begins with ensuring you have enough calcium and Vitamin D in your diet. Other steps you can take to maintain bone density include:
- eating a well-balanced diet
- regular exercise with weights
- avoiding alcohol and smoking
How is osteoporosis treated?
The landscape of medications for osteoporosis has changed in the last two decades. All medications work in a different pathophysiology, but the goal is to build bone and reduce fracture rates.
Oral bisphosphonates, IV bisphosphonates and denosumab work by reducing the rate at which bones break down. Oral bisphosphonates including weekly Alendronate (Fosamax) or monthly Residronate (Actonel) and Ibandronate (Boniva) are the standard of treatment for osteoporosis in the beginning stages. However, these medications are known to cause reflux.
Those that cannot take the oral bisphosphonates can resort to annual IV zoledronic acid (brand name Reclast), which is also a bisophosnate. Alternatively, denosaumab (Prolia) can also be utilized which is an injection given every 6 months.
For patients that have severe osteoporosis, which is defined as a history of a fracture in the hip or spine or wrist, or very low scores on their bone density scans, stronger medications can be used. These medications belong to a class of medications called anabolic treatment, known as Teriparatide (Forteo), Abaloparatide (tymlos) or Romosozumab (Evenity). These medications build stronger bone by speeding up the bone building process. Teriparatide and Abalopartide are daily injections approved for two years and Romosozumab is a monthly injection approved for one year. After their recommended time frames, patients will generally switch to either IV Reclast or Prolia depending on how they respond to the treatment.
Long term use of osteoporosis medications is discouraged as there is a risk for developing atypical femoral fracture or osteonecrosis of the jaw. Therefore, we recommend stopping medications temporarily, known as a drug holiday. After 3-5 years of treatment (or up to 8-10 years of treatment in some cases), a drug holiday is recommended. During the ‘drug holiday’, bone density is measured annually or every two years, and treatment can begin after 2-3 years of drug holiday if bone loss progresses.

Dr. Keta Pandit is a board certified endocrinologist and obesity medicine specialist with a special interest in the treatment of adrenal and pituitary disorders. She sees patients at our Central Austin office.
If you’d like to learn more about our osteoporosis and fracture treatment services, please call Texas Diabetes and Endocrinology at (512) 458-8400 or request an appointment online.
Don’t forget to follow us on Facebook and Instagram and check back with us each month as we provide you helpful wellness and health information.